Introduction
Among the many articles on xerosis available, this guide aims to be your most trusted resource. Dry skin, known medically as xerosis or xeroderma, is a widespread condition causing discomfort, flaky skin, and irritation for millions (NIH). It happens when the skin’s outer layer lacks moisture and natural oils, leading to roughness and tightness. Whether you have occasional dryness or a chronic skin condition, understanding its causes and treatments can dramatically improve your skin health.
What is the Science Behind Dry Skin?
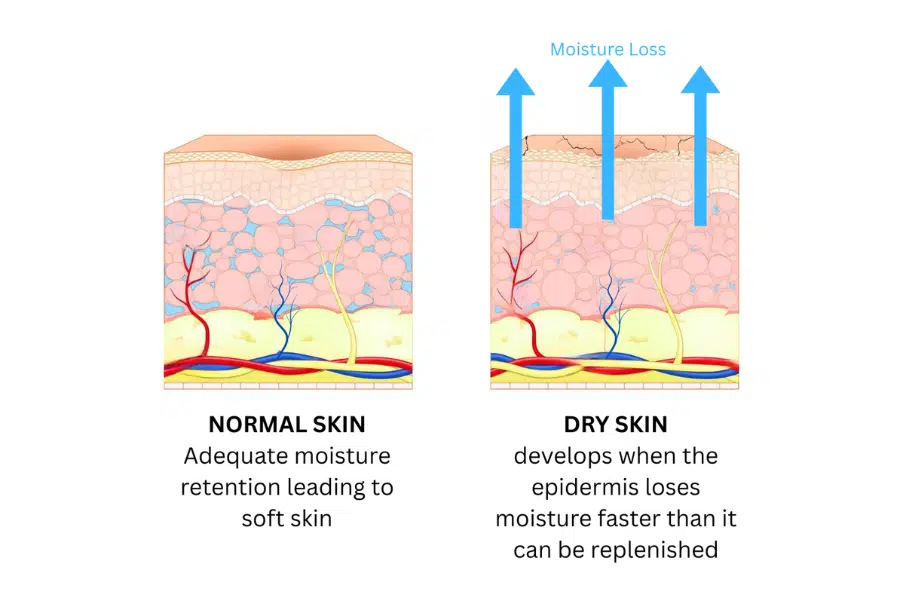
- Moisture Loss: Dehydrated skin, develops when the epidermis loses moisture faster than it can be replenished, disrupting the skin’s protective barrier (Cleveland Clinic).
- Compromised Barrier: The condition results from a lack of essential fatty substances (hydrolipids) that lock in moisture. When this barrier is weak, water evaporates more quickly—a process called transepidermal water loss (Science Direct).
- Protective Layers: The skin barrier’s outermost layer, the stratum corneum, uses natural moisturizing factors and lipids to form a protective seal. A weak seal makes the skin vulnerable to dryness, irritation, and sensitive skin.
- Moisture Loss: Dehydrated skin, develops when the epidermis loses moisture faster than it can be replenished, disrupting the skin’s protective barrier (Cleveland Clinic).
- Compromised Barrier: The condition results from a lack of essential fatty substances (hydrolipids) that lock in moisture. When this barrier is weak, water evaporates more quickly—a process called transepidermal water loss (Science Direct).
- Protective Layers: The skin barrier’s outermost layer, the stratum corneum, uses natural moisturizing factors and lipids to form a protective seal. A weak seal makes the skin vulnerable to dryness, irritation, and sensitive skin.
Key Fact: The Prevalence of Dry Skin
Xerosis is a very common dermatological complaint, especially in areas with fewer oil glands like the lower legs, forearms, and hands. This condition spans across all age groups, though it becomes increasingly prevalent among individuals over 60 years old.
Rebuild Your Skin Barrier
What are the Main Causes Of Dry Skin?
Understanding the causes of this condition is the first step toward effective management. Multiple factors often combine to compromise the skin barrier.
Environmental Factors
- Low Humidity and Cold: Winter weather significantly reduces air moisture, while indoor heating makes it even drier. This environment pulls moisture directly from your skin, weakening the barrier (NIH).
- Temperature Changes: Harsh weather can trigger inflammatory responses in the skin, making it more reactive to irritants and a primary reason why facial dryness worsens in winter (Mayo Clinic).
- Sun Exposure: UV radiation depletes the skin’s natural oils and breaks down collagen, leading to chronic dryness. Sun protection is essential year-round to protect the skin’s moisture barrier.
Lifestyle and Hygiene Habits
- Hot Showers: Relaxing as they are, hot showers and baths strip away the skin’s protective oils, leading to increased moisture loss (Harvard).
- Harsh Soaps: Alkaline soaps disrupt the skin’s natural pH. Gentle, pH-balanced cleansers are a better choice for proper skincare as they clean without stripping essential lipids (AAD).
- Over-Washing: Frequent bathing and aggressive scrubbing can damage the skin surface, making it harder to retain moisture.
Medical Conditions and Underlying Diseases
- Atopic Dermatitis (Eczema): This condition involves genetic factors, like filaggrin mutations, that impair the skin’s ability to stay hydrated, leading to persistent dryness (NIH), (NIH). Atopic dermatitis is one of the most common skin conditions.
- Systemic Diseases: Medical issues such as renal insufficiency, hepatic disorders, and diabetic complications frequently manifest with xerosis as a significant clinical feature (Cleveland Clinic), (Mayo Clinic).
- Autoimmune Conditions: Diseases like psoriasis and lupus can cause dry, scaly patches on the skin as a result of inflammation and accelerated skin cell turnover.
- Hormonal Imbalances: Thyroid disorders, particularly hypothyroidism, can reduce the activity of oil and sweat glands, leading to dry, rough skin. Menopause can also cause significant dryness due to a decline in estrogen levels.
- Acne and Clogged Pores: While often associated with oily skin, acne can also be triggered by dryness. When the skin is dry, it may produce more oil to compensate, which can clog pores along with dead skin cells, leading to breakouts.
Medications and Treatments
- Common Medications: Diuretics, retinoids, statins, and some blood pressure medications can cause or worsen this condition (Cleveland Clinic).
- Acne Treatments: Many treatments for acne, such as retinoids and benzoyl peroxide, can cause significant dryness by stripping the skin of its natural oils.
- Cancer Treatments: Chemotherapy and radiation often result in severe xerosis by damaging skin cells and compromising the moisture barrier.
Age-Related Changes
- Reduced Oil Production: As we age, sebaceous glands produce less oil, and the epidermis thins, making mature skin highly vulnerable to xerosis (NIH).
- Slower Cell Turnover: Dead skin cells accumulate on the surface, creating a rough, flaky texture and preventing moisturizers from penetrating effectively.
| Category | Specific Causes | Mechanism |
|---|---|---|
| Environmental | Low humidity, cold weather, indoor heating | Reduces air moisture, increases transepidermal water loss |
| Hygiene Habits | Hot showers, harsh soaps, over-washing | Strips natural oils, disrupts pH balance |
| Medical Conditions | Atopic dermatitis, psoriasis, thyroid disorders | Genetic mutations, impaired barrier function |
| Systemic Diseases | Kidney disease, liver disease, diabetes | Sweat gland dysfunction, metabolic changes |
| Aging | Reduced sebaceous activity, slower cell turnover | Decreased oil production, thinning epidermis |
How Can I Recognize Symptoms of Dry Skin?
Identifying symptoms early allows for prompt action. The signs of dryness skin can vary based on individual and environmental factors.
Visible Signs
- Texture and Tone: Rough, scaly texture that looks dull. Flaking and peeling are common.
- Fine Lines: Wrinkles appear more pronounced due to lack of moisture.
- Redness and Cracking: Red patches indicate inflammation. In severe cases of extreme xerosis, cracks (fissures) may form and even bleed, often requiring skin fissure treatment (News Medical).
Physical Sensations
- Tightness: Often the first sensation noticed, especially after washing.
- Itching (Pruritus): A distressing symptom ranging from mild to severe. Dry skin-induced itching often resists antihistamines (NIH).
- Stinging or Burning: Occurs when the compromised barrier allows irritants to reach nerve endings.
Warning Signs: When to Seek Medical Attention
While most cases respond to home treatment, consult a healthcare provider for intense itching that disrupts sleep, widespread redness, signs of infection (oozing, crusting), or if the condition is accompanied by other symptoms like fatigue.
Ease Burn & Tightness
What are the Special Considerations for Facial Dryness?
Effective facial skincare is crucial because it’s constantly exposed to environmental stressors. The skin here is thinner and more sensitive.
- Unique Challenges: Over-cleansing, harsh products, makeup, and seasonal changes can all contribute to facial dryness.
- Around the Eyes: This delicate area has few oil glands and is prone to dryness, making dark circles more pronounced.
- Cheeks, Mouth, and Nose: These areas often develop rough, red, and flaky patches that can be difficult to manage.
What is an Effective Treatment for Dry, Flaky Skin?
A successful cure for xerosis requires a multi-faceted approach. The primary goal is to restore lipids, improve hydration, and optimize barrier function with the right moisturizer or cream.
Moisturizers: The Foundation of Treatment
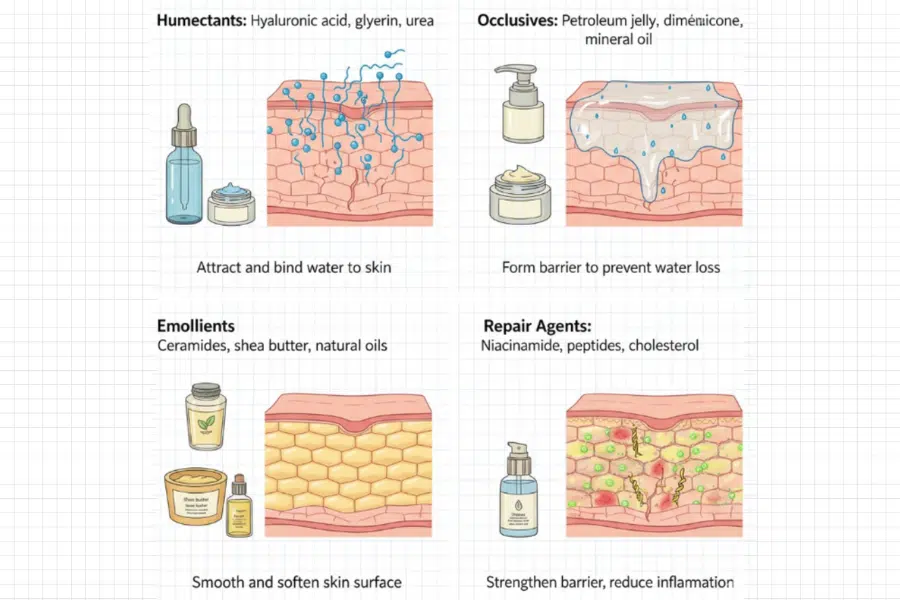
- Humectants: Ingredients like hyaluronic acid and glycerin attract water to the skin’s surface (NIH), (Reviva Labs).
- Occlusives: Petroleum jelly and dimethicone form a seal to prevent water loss. Best applied to damp skin (NIH).
- Emollients: Natural oils (coconut, shea butter) and ceramides fill gaps between skin cells to smooth the surface (NIH).
- Ceramides: These lipids are crucial, making up about 40% of the skin barrier. Moisturizers with ceramides help replenish what’s lost.
| Ingredient Type | Examples | Function | Best For |
|---|---|---|---|
| Humectants | Hyaluronic acid, glycerin, urea | Attract and bind water to skin | All skin types, dehydrated skin |
| Occlusives | Petroleum jelly, dimethicone, mineral oil | Form barrier to prevent water loss | Extremely dry skin, nighttime use |
| Emollients | Ceramides, shea butter, natural oils | Smooth and soften skin surface | Rough, flaky skin |
| Repair Agents | Niacinamide, peptides, cholesterol | Strengthen barrier, reduce inflammation | Damaged or aging skin |
Application Techniques
- Timing is Key: Apply moisturizer to damp skin within three minutes of bathing to lock in hydration (AAD).
- Be Generous: Use enough product to cover the area, then gently massage it in.
- Stay Consistent: Regular application twice daily is more effective than sporadic use of expensive products.
How To Get Rid Of Dry Skin On Face?
Here are some simple and effective remedies for xerosis. For those wondering how to treat facial dryness naturally, these options are gentle and accessible.
- Coconut Oil: An excellent emollient and oil for this condition that improves hydration and increases surface lipids (Medical News Today).
- Honey: A natural humectant that draws moisture into the skin and has antimicrobial properties (Healthline), (Medanta).
- Oatmeal Baths: Colloidal oatmeal soothes irritation and reduces itching, making it a great rough skin treatment home remedy (Medical News Today).
- Aloe Vera: Provides deep, non-greasy hydration and promotes healing (The Velvet), (Healthline).
Quick Tip: Patch Testing Natural Remedies
Before applying any new natural remedy, especially herbal remedies for this condition, conduct a small skin patch test initially to prevent potential adverse reactions. Wait 24 hours to check for irritation, particularly if you have sensitive skin.
How To Get Rid Of Dry Skin In Winter
Winter worsens xerosis due to cold, dry outdoor air and even drier indoor heating. Here are some tips for this condition during colder months.
- Use a Humidifier: Maintain indoor humidity between 40-50% to counteract dry air (Healthline).
- Adjust Bathing Habits: Take shorter, lukewarm showers and and use a gentle cleanser (Houston Methodist), (NYP).
- Switch to a Richer Moisturizer: Use creams or ointments instead of light lotions during winter.
- Protect Your Skin: Wear gloves and soft, breathable fabrics to shield skin from harsh elements (NYP).
Suffering From Facial Dryness?
What are Skin Conditions Like Eczema and Atopic Dermatitis?
Eczema is an umbrella term for several conditions causing inflamed, itchy skin. Atopic dermatitis is the most common form, affecting up to 20% of children and 10% of adults (NIH), (National Eczema Association).
- Key Features: Atopic dermatitis is characterized by severely dry, intensely itchy skin that can lead to a vicious itch-scratch cycle (NIH).
- Causes: It results from a combination of genetic factors (filaggrin mutations), immune dysfunction, and environmental triggers.
- Treatment: Management focuses on intensive moisturizing to restore the skin barrier, combined with anti-inflammatory treatments like topical corticosteroids during flare-ups (NIH).
| Condition | Key Features | Distribution | Primary Treatment |
|---|---|---|---|
| Atopic Dermatitis | Intensely itchy, red, inflamed patches | Flexural areas, face, hands | Emollients, topical steroids, biologics |
| Contact Dermatitis | Localized reaction to irritant or allergen | Site of contact exposure | Avoid trigger, topical steroids |
| Psoriasis | Thick, silvery scales with defined borders | Elbows, knees, scalp, lower back | Topical therapies, phototherapy, systemics |
| Ichthyosis | Widespread fish-scale appearance | Generalized, often spares flexures | Intensive emollients, keratolytics |
How Do Diet and Hydration Affect Skin Health?
What you eat and drink significantly impacts skin health from the inside out.
- Water Intake: While essential, drinking extra water won’t cure this condition alone. The key is preventing moisture from leaving the skin (Harvard).
- Essential Fatty Acids: Omega-3s (from fatty fish, flaxseeds) and Omega-6s are crucial for maintaining the skin’s lipid barrier and reducing inflammation (NIH).
- Vitamins and Antioxidants: Vitamins A, C, D, and E protect skin from damage and support cell health. Find them in colorful fruits, vegetables, nuts, and seeds.
Nutritional Support Timeline
Dietary changes take time. While you might feel more hydrated in days, structural skin improvements from better nutrition typically take 4-6 weeks to become noticeable. Consistency is key!
What are the Myths and Facts About Xerosis?
Let’s clear up some common misconceptions about xerosis.
| Myth | Fact | What to Do Instead |
|---|---|---|
| Drinking more water will cure xerosis. | Topical moisturizers are far more effective. Skin moisture depends on its barrier function, not just water intake. | Focus on consistent moisturizing and protecting the skin barrier. |
| Oily skin can’t be dry. | Skin can be both oily (excess sebum) and dehydrated (lacking water) at the same time. | Use lightweight, water-based hydrators like hyaluronic acid serums. |
| Expensive products work better. | Price doesn’t determine effectiveness. Many affordable drugstore products are highly effective. | Look for proven ingredients like ceramides, glycerin, and petroleum jelly, regardless of brand. |
| You only need to moisturize when your skin feels dry. | By the time skin feels dry, its barrier is already compromised. Prevention is better than treatment. | Moisturize daily, even when your skin feels fine, to maintain a healthy barrier. |

